Hi all. Welcome to post 57 in the Strength & Conditioning For Therapists blog series, and part 2 on Whole Body Vibration (WBV). Last time we looked at what WBV was, addressed some of the pertinent methodological issues and its safety. Here we’re going to look at a bit of the evidence base for Whole Body Vibration in rehabilitation. Enjoy.
Applications of Whole Body Vibration in Rehabilitation
Type “whole body vibration rehabilitation” into PubMed and you’ll get around 750 results. It’s a widely researched method in clinical populations; here are just some of the applications investigated;
- Children with cerebral palsy
- Stroke rehab
- Ankle instability
- COPD
- Bone health in post-menopausal women
- Low back pain
- Post ACL reconstruction
- Knee osteoarthritis
- Falls prevention
- … and more
As we covered last week, the ability of the (correctly-dosed) WBV stimulus to activate the musculature, without the requirement to lift heavy weights, is an appealing modality in load- and neurologically-compromised populations. With the appropriate frequency (of WBV stimulus) and duration of exposure, research shows that we can positively affect muscle strength, proprioception and function. So how do we do it?
Whole Body Vibration in Rehabilitation
If we look at all clinical applications, we’d be here forever. So, let’s just pick knee osteoarthritis (OA) for now, but be mindful that there are evidence-based recommendations and positive outcomes for other clinical groups. I’ve posted a link to a systematic review and meta-analysis on the effects of WBV in children with cerebral palsy in the references below as an example.
Whole Body Vibration Training and Knee Osteoarthritis
I think it’d be good here to pull out a few studies and compare their protocols and findings. I think by now, you should be able to critique their interventions, reflecting back on some of the fundamental principles of exercise prescription: Specificity, Overload, Progression.
To make these comparisons easier, I’ve tabularised the key methodological details for each of the 3 studies. Let’s go.
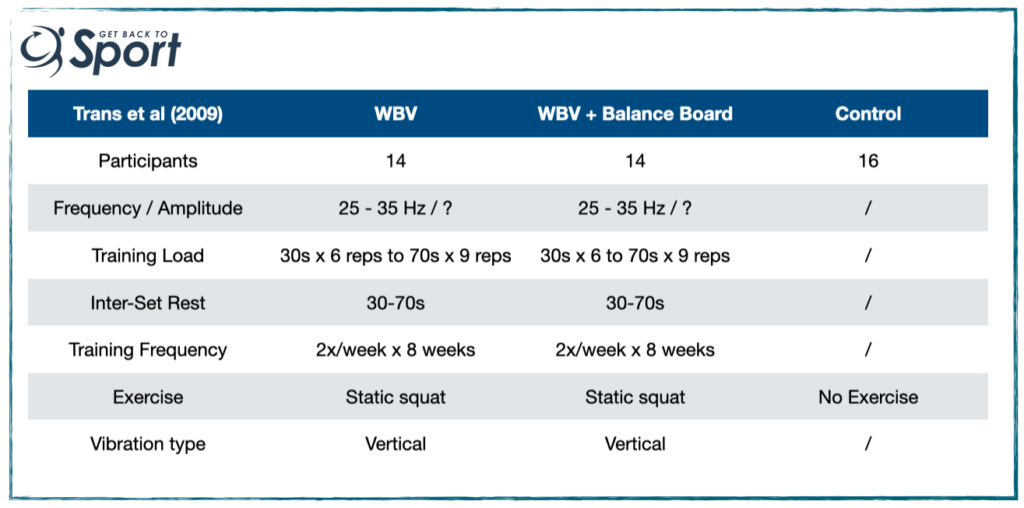
So Trans et al. (2009). recruited 52 females with knee OA (60.4 yrs) and randomly-assigned them to one of 3 conditions WBV; WBV with balance board built in, or a no exercise control. See the table below for their protocol.
Findings:
- Approximately 12% increase in isometric & isokinetic torque in the exercise groups (no change in control or difference between exercise groups)
- 30% change in threshold to detection of passive motion in the exercise groups (no change in control)
- No change to self-reported outcomes (WOMAC)
Some Questions?:
- Is 12% a decent level of change for 16 sessions?
- Was the training load / prescription specific enough to optimise strength gains? [up to 70 seconds os sustained effort, with up to 70 seconds rest]
A few years later, we have a study by Tsuji et al. (2014). Again they recruited women (50-73yrs) with knee pain and radiographically-verified knee OA and randomly allocated them into a WBV or control condition. Here’s their protocol:
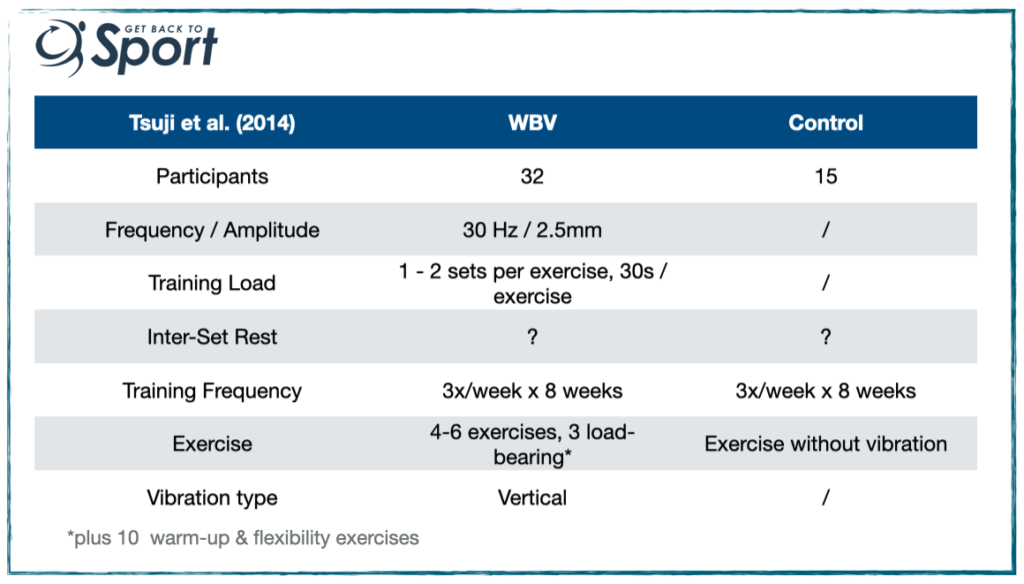
Findings:
- Effect sizes (ES) of 0.48 – 0.72 of pre- to post change in isometric and isokinetic strength and in perceived & functional outcomes (ES of 0.48 – 0.72 means here roughly 66% – 79% of people in the exercise group have superior performance post exercise compared to pre). But …
- No significant differences in strength changes between groups.
Questions?:
- How much rest was given between sets? This is important, right? (see here for a post I wrote about rest and recovery)
- 30Hz – Might a higher frequency elicited a better response? Vertically vibrating plates require a greater vibration frequency to elicit the same level of muscle activation compared to side-oscillating plates. High frequencies on vertical plates are less well tolerated though.
- Again, can we comment on the exercise prescription …?
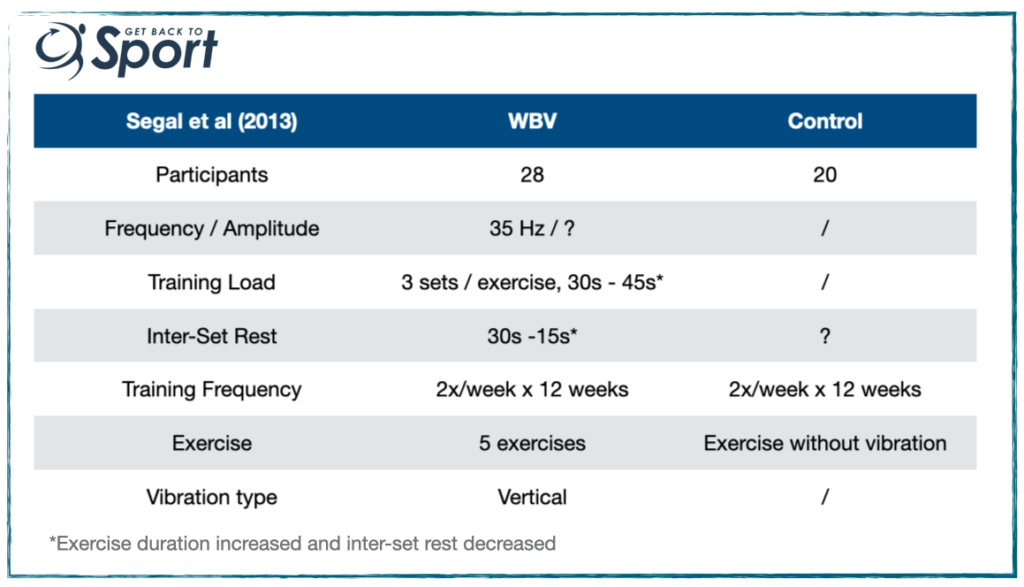
Here we have a final study to review by Segal et al (2013). They recruited 48 women (45 – 60 yrs) with knee OA and randomly-allocated them into a WBV or control condition.
Findings:
- No change to isokinetic strength, but a small increase in leg press strength of around 8%, which was similar between groups.
Questions?
- It appears as thought WBV is no better than static squatting in eliciting strength changes, if any.
- Is 8% increase in leg press strength a reasonable amount over 24 sessions?
- Looking at the exercise prescription, progression was described by an increase in duration of squat and a decrease in rest period. Are you questioning the specificity of the intervention? I am.
Is Whole Body Vibration Good For OA?
Okay, so what can we say about WBV in (female) OA populations. We may be thinking that it might be good in an OA population which is load-compromised, i.e. they can’t tolerate moderate to heavy loads. Perhaps based on the above evidence we shouldn’t expect huge gains in strength and, o,r function, and maybe in some circumstances it might not outperform standard and static exercise prescription. Hmmm.
Or, do you see something else…?
What about if we apply our critical thought about the principles of training, specificity and muscle fatigue in our review of the above exercise prescriptions? Do you think that if the key outcome was to improve muscle strength then reps of 30-70 seconds with minimal inter-set rest could be improved upon?
In fact, if you go back and look at the exercise prescriptions, can you predict what the specificity of each exercise prescription was? I’ve provided the links to the abstracts and papers, where possible below so you can test your predictions and further critique the papers. Let me know what you find!
Summary
So, what do we think about whole body vibration in rehabilitation settings? As I said, we’ve just taken a very small snapshot of its application in rehab here, but hopefully provided you with some food for thought.
My opinion? I think WBV is a great tool – providing you use the right tool (not cheap, unregulated devices from the internet!) for load- and neurologically-compromised populations. There’s far more research we can look at here- perhaps another time. I also think that standard exercise prescription can be honed far better to elicit the desired outcomes of the session / programme / training cycle. Indeed, I and my collaborators have done this with great effect in rehab settings.
Let me know your thoughts – have you experience in using WBV, have you critiqued the studies mentioned (or others)? What’s your opinion?
Thanks for reading. Until next time…
References
- Saquetto et al. (2015). The effects of whole body vibration on mobility and balance in children with cerebral palsy: a systematic review with meta-analysis. J Musculoskelet Neuronal Interact. 15(2):137-44 [Full Paper LINK]
- Trans et al. (2009) The Knee 16; 256–261[Abstract LINK]
- Tsuji et al. (2014). The Knee 21: 1088–1095 [Abstract LINK]
- Segal et al. (2013). PM R; 5:201-209 [Full Paper LINK]
Recent Comments